- Induced/adaptive human T regulatory cells generated from peripheral CD4 cells
- Confirmed suppressive capacity
- Used for a wide variety of in-vitro applications, including co-culture suppression and cytotoxicity assays
- Carefully cryopreserved to ensure high viability (> 80%) upon thawing
- All orders come with an iQ Certificate of Analysis
- Normally ships out same business day
Human Induced T Regulatory Cells
$515.00
Description
Human T Regulatory Cells
Human T regulatory cells (Treg cells) are characterized as CD4+ lymphocytes cells that can negatively regulate the activity of T cells, B cells, NK cells, and macrophages. Their suppressive function in lymphoid and non-lymphoid tissues help to establish and maintain tolerance to prevent autoimmunity and hyper-activation in inflammatory responses. Numerous studies have demonstrated the role of Treg cells in the development of autoimmune diseases and efforts are underway to target them with therapeutics to treat these diseases.
Recent studies have also shown that Tregs can infiltrate and develop in the tumor environment. Ovarian, renal, and colon cancers are among the human cancers that have been linked to increased Tregs. Not surprisingly, poor prognosis is associated with an increase in the number of these cells. With these emerging findings, researchers are developing therapeutics that specifically target Tregs to eliminate them from the tumor environment so that remaining lymphocytes can become activated and target tumor cells.
Treg cells come in various subtypes and can develop in the thymus or periphery. Those that develop in the thymus are called Natural Tregs (nTregs), while those that develop in the periphery and tumors are termed Induced Tregs (iTregs). Interestingly, studies have demonstrated that iTregs are more potent at regulating function compared to nTregs. In addition, iTregs can be generated in vitro using a combination of cytokines that drive conventional CD4 cells into iTregs. Both nTregs and iTregs express the surface proteins CD4 and CD25, as well as the transcription factor FOXP3. An additional criteria to identify both types of Tregs is the low expression of CD127, the IL-7 receptor.
Finally, Tregs can suppress lymphocyte function through multiple mechanisms. They can secrete immuno-suppressive factors, such as IL-10 and TGF-b, to prevent the activation or down-regulate the activity of lymphocytes. They may also work by being an “IL-2 sink” in which the high expression of the IL-2 receptor on Tregs bind the local concentrated amount of IL-2 to prevent it from binding lymphocytes to drive an inflammatory response. In addition, Tregs may express checkpoint proteins, such as CTLA-4 and PD-L1, to act through cell-cell contact.
Application Summary for Induced T Regulatory (iTreg) Cells
Induced Tregs are a good source of cells to study the function of Tregs in an in vitro setting, in particular co-culture suppression assays. Here, Tregs are co-cultured with lymphocytes and then assayed for lymphocyte proliferation and cytokine release. In the presence of Tregs, lymphocyte function should be down-regulated.
With the current trend towards development of molecules that modulate the immune system to treat cancer and autoimmune diseases, these co-culture assays are also commonly used to test whether a potential therapeutic can inhibit or promote Treg function. Further, because Tregs are difficult to isolate from tissue and a great number of them are required for co-culture assays, frozen induced Tregs are a valuable source to enable the execution of these studies.
For some antibody-based cancer therapeutics being developed, Tregs are being targeted for antibody-dependent cellular cytotoxicity or complement dependent cytotoxicity. Therefore, frozen iTregs are also a good source of target cells for these studies interrogating cell death.
Many questions about how iTregs develop and progress through developmental stages also remain unanswered, and frozen iTregs are a good source of cells to study this development through genetic and transcriptional profiling. DNA or RNA can easily be isolated from these cells and used for downstream applications and analysis.
Induction/Generation of iTregs
Naive CD4 cells isolated from PBMCs underwent a proprietary process under sterile conditions to generate iTregs. To ensure that Tregs were induced, cells are analyzed for the expression of CD4, CD25, and CD127 (Figure 1). Therefore, our frozen iTregs are a reliable and ideal source to obtain plentiful cells for your studies.
Purity and Function
A small aliquot of cells was analyzed for differentiation into Treg cells by flow cytometry analysis. Characterization of iTreg cells, as defined by CD4 and CD25 expression, was > 94% (Figure 1). Our iTreg cells are also verified by low CD127 expression and confirmed as functionally suppressive.
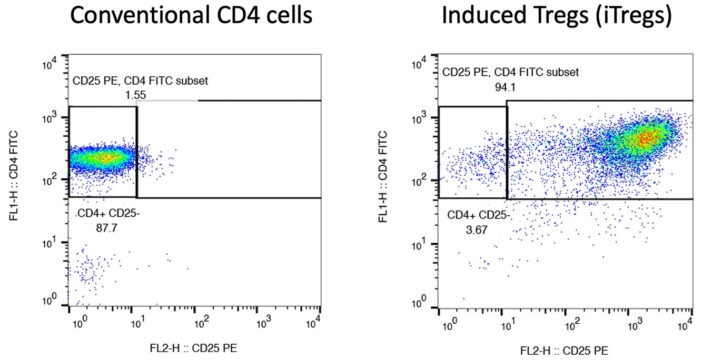
Figure 1. CD4 and CD25 expression after conversion from conventional CD4 cells. Conventional CD4 (left) cells were converted into iTregs (right) using a proprietary method. A small aliquot was taken after induction to evaluate expression of CD4 and CD25 by flow cytometric analysis (right).
Cryopreservation and Storage
Our iTregs were cryopreserved carefully using iQ Biosciences’ cryopreservation protocol that ensures high viability (> 80%) after thawing.
Cells should be stored at < -120°C once they are received, such as within a liquid nitrogen tank (vapor phase).
Quality Control Process
We implement random sampling per lot to test for viability and cell counts to ensure they meet specifications, which are recorded on the Certificate of Analysis that is included with each shipment. Cell counts are obtained using a manual hemocytometer and then cross-referenced with an automated cell counter. Each lot is also characterized for unique cell populations by immunophenotyping, in which the results are also recorded on the Certificate of Analysis.
Additional information
| Available Size(s) | |
|---|---|
| Cell Type | |
| Format | |
| Species | |
| Tissue Type | |
| Viability | > 80% |
We are Committed to Ethical Practices
iQ Biosciences’ human primary cell products are lawfully obtained in accordance with Local, State, and Federal U.S. requirements, and the collection of cells complies with ethical requirements. Our cells are obtained from normal or disease patient volunteers participating in a donor program that is approved by an Institutional Review Board (IRB) or Human Subject Committee. A signed and witnessed consent form is obtained from donor volunteers prior to starting the collection protocol. Strict controls on personal identifiers of volunteers are in place in order to protect their privacy.
For US customers, we ship via FedEx Overnight Shipping. Shipping charges will vary per shipping address (based on ZIP code) and are estimated to be $140.
For international (non-US) customers, we work closely with you and our couriers to ensure all necessary documentation is in place for international shipments to significantly reduce the chance of delays at Customs. For the export of non-human primate samples, this includes preparing CITES permits, as well as any other documentation as required by country. Please submit an inquiry to orders@iqbiosciences.com for your estimated time of delivery and shipping charges.
Austria
Hölzel Diagnostika Handels GmbH
Tel: +49 221 126 02 66
Email: info@hoelzel.de
Web: https://www.hoelzel-biotech.com/
Canada
Cedarlane
Tel: +1 (289) 288-0001
Toll Free (North America): +1 (800) 268-5058
Fax: +1 (289) 288-0020
Email: sales@cedarlanelabs.com
Web: https://www.cedarlanelabs.com
China
BIOHUB INTERNATIONAL TRADE CO., LTD.
上海起发实验试剂有限公司
Address: Chuansha Rd #6619, Pudong, Shanghai, Zipcode: 201200 P.R.China
Tel: 0086-021-50724187
Phone: +86-15921799099
Fax: 0086-021-50724961
Email: sale3@78bio.com
Web: www.qfbio.com
European Union
Caltag Medsystems Ltd.
Email: office@caltagmedsystems.co.uk
Web: https://www.caltagmedsystems.co.uk
tebu-bio
Web: https://www.tebu-bio.com
Or Find a local contact
Germany
Hölzel Diagnostika Handels GmbH
Tel: +49 221 126 02 66
Email: info@hoelzel.de
Web: https://www.hoelzel-biotech.com/
Zageno
Web: https://zageno.com/
Ireland
2B Scientific Ltd
Tel: +44(0) 1869 238033
Fax: +44(0) 1869 238034
Email: sales@2BScientific.com
Web: https://www.2bscientific.com
India
Cell & Gene BioSolutions Pvt. Ltd.
#478 C, SLV Complex, Raghavendra Swamy Mutt Road
Opp. Turahalli Water Tank, Turahalli, Subramanyapura Post
Uttarahalli Hobli, Bengaluru-560061, Karnataka, India
Phone: +91 97317 14670
Phone: +91 98809 25033
Email: info@cgbios.com
Web: www.cgbios.com
Japan
Cosmo Bio Co., Ltd.
Tel: +81 (03) 5632 9610
Fax: +81 (03) 5632 9619
Email: nsmail@cosmobio.co.jp
Web: https://www.cosmobio.co.jp
Qatar
Sedeer Medical Services and Trading LLC
Tel: +974 4434 9191
Email: info@sedeer.com
Web: https://sedeer.com/
Singapore
Omnicell Pte Ltd
Tel: +65 6747 0201
Email: enquiry@omnicell.com.sg
Web: https://omnicell.com.sg/</a
South Korea
BioClone
Tel: +82-2-2690-0058
Email: bioclone@bioclone.co.kr
Web: http://www.bioclone.co.kr
Switzerland
Hölzel Diagnostika Handels GmbH
Tel: +49 221 126 02 66
Email: info@hoelzel.de
Web: https://www.hoelzel-biotech.com/
Taiwan
Hycell International Co. Ltd.
Tel: +886-2-2877-1122
Fax: +886-2-2876-1520
Web: http://www.hycell.com.tw
United Kingdom
2B Scientific Ltd
Tel: +44(0) 1869 238033
Fax: +44(0) 1869 238034
Email: sales@2BScientific.com
Web: https://www.2bscientific.com
Caltag Medsystems Ltd.
Tel: +44 (0)1280 827460
Fax: +44 (0)1280 827466
Email: office@caltagmedsystems.co.uk
Web: https://www.caltagmedsystems.co.uk
tebu-bio
Tel: +44 (0)1733 421880
Fax: +44 (0)1733 421882
Email: uk@tebu-bio.com
Web: https://www.tebu-bio.com
Zageno
Web: https://zageno.com/
United States
Fisher Scientific
Tel: 1-800-766-7000
Web: https://www.fishersci.com
Quartzy
Web: https://www.quartzy.com
VWR International
Tel: 1-800-932-5000
Web: https://www.vwr.com
Zageno
Web: https://zageno.com/